Comparative Study of Fresh Embryo Transfer versus Frozen Embryo Transfer in IVF/ICSI on The Basis of Patient Age
Dr Vikram Singh Bhati
DOI10.36648/2476-2008.2021.6.17
Bhati VS*
Virk Fertility Services, Jalandhar, Punjab, India
Received Date: February 16, 2021; Accepted Date: February 28, 2021; Published Date: March 18, 2021
Citation: Bhati VS (2021) Comparative Study of Fresh Embryo Transfer versus Frozen Embryo Transfer in IVF/ICSI on The Basis of Patient Age. J Rep Endo Infert. Vol.6 No.2:17.
Abstract
Objective: To evaluate the available evidence to assess cryopreservation of all embryos or subsequent frozen embryo transfer (FET) results compared with fresh embryo transfer.
Design: Systematic review and pregnancy outcome ratio.
Setup: Virk Fertility Services Jalandhar, Punjab. IVF lab for reproductive care. Patient(s): Infertility patient(s).
Intervention(s): We included randomized clinical trials comparing outcomes of IVF cycles between fresh and frozen embryo transfers for almost 422 patients.
Main Outcome Measure(s): The outcomes of interest were ongoing pregnancy rate, clinical pregnancy rate.
Result(s): We included three trials accounting for 422 cycles in women aged 20–45 years. Data analysis showed that FET resulted in significantly higher ongoing pregnancy rates and clinical pregnancy rates.
Conclusion(s): Our results of 422 patients showed that frozen embryo transfer can give better pregnancy outcome in 31-45 age group patient. Because by FET we can maintain time gap between the endometrium and embryos transfer. And we can overcome the adverse effects of controlled ovarian hyper-stimulation (COH) on ER during ART cycles.
Keywords
Fresh embryo transfer; Frozen embryo transfer; Endometrial receptivity; Pregnancy outcome
Introduction
Assisted reproductive technology (ART) involves handling of gametes (eggs and sperm cells) or embryos outside the human body with the goal to achieve pregnancy leading to the birth of a healthy child. The most widely used treatment for subfertility is in vitro fertilization (IVF) with or without intracytoplasmic sperm injection (ICSI) followed by the transfer of one or more embryos into the triple layer of uterus. When there are additional embryos they are frozen, allowing them to be used in a future cycle should the couple not conceive from the fresh transfer or to be used later if the couple wishes to have another child. In Vitro Fertilization (IVF) or Intra Cytoplasmic Sperm Injection (ICSI) treatment cycles often produce more embryos than we can be transferred 2-3 good embryo during the fresh treatment cycle. Embryo implantation represents one of the important steps for the success of assisted reproduction techniques (ART) [1]. Its effectiveness depends upon three main parameters: embryo quality, endometrial receptivity (ER), and a well-balanced embryo endometrium interaction [2]. Many times, in some patients embryo transfer is postponed for medical reasons (e.g. ovarian hyper-stimulation syndrome). Cryopreservation of these embryos provides both physicians and patients a safe, successful and cost-efficient option [3,4]. The implantation window is a self-limited period in which the endometrium has develop the adequate morphologic and functional state for the embryo attachment. Therefore, ER is essential for conceptionin natural and infertilitytreatment cycles. However, it has been observed in past research that controlledovarian hyper-stimulation (COH) adverselyaffects ER during ART cycles [5,6]. This interaction is mediated by the supra-physiologic levels of estradiol (E2) and progesterone (P) during the follicular phase leading to morphologic and biochemical endometrial alterations and a more advanced endometrium than in natural cycles. These physiologic changes may affect the success rates of the treatments. This altered hormone level could be controlled by giving time gap between the endometrium and transferred embryos for that purpose we would use the technique called frozen embryo transfer. Pregnancy rates after frozen-thawed embryo transfer are high compare to pregnancy rates after fresh transfer.
Objective
To determine pregnancy rate with frozen-thawed embryo transfers has a positive effect on fertility outcomes, including live birth rate, compared to standard IVF with fresh and frozen-thawed embryo transfers as according to patient age group. The purpose of the present systematic study was to examine the comparative result of cryopreservation of all good quality embryos, and subsequent FET, is associated with improvements in the pregnancy outcomes compared with fresh embryo transfer.
Material and Methods
Now in these days IVF & ICSI cycles are characterized by controlled ovarian stimulation (COS) for obtaining multiple oocytes for ICSI [7]. Subsequently, fresh transfer of best embryo is performed, in this fresh embryo transfer so, many women fail to achieve a pregnancy after transfer of one or more fresh embryos. Recent development in cryopreservation have led to increased chances of embryo survival after frozen thawed embryo transfer pregnancy outcome is increased [8]. In this frozen thawed embryo transfer strategy where no fresh transfer is conducted and all available embryos are cryopreserved and thawed and transferred in a subsequent cycle without ovarian hyper-stimulation [9,10]. In frozen embryo transfers (FET), endometrial priming may be achieved with the use of E2 and P, and the endometrial development can be controlled more precisely than in cycles of COH with gonadotropins [11,12].
Steps of Study and Participants
In this cross sectional study 422 ICSI-ET cycles (210 fresh ET and 222 FET) were observed. 422 women undergoing ICSI treatment referred to Virk Fertility Services, Jalandhar, Punjab, India from 2015 to Aug 2016 were reviewed. Our focus area of study was: ICSI and IVF treatment using Flexible antagonist protocol. Endometrial thickness more than 8 mm, and having normal follicle stimulating hormone (FSH) of the third day of menstrual cycle. The women with natural cycles, and women those have any history of hypothyroidism and hyperthyroidism, and hyperprolactinemia, history of surgical removal of endometriosis, leiomyoma, uterine septum, were excluded.
Following parameters were measured
Maternal and paternal age at the time of embryo transfer, patient history like numbers of child, duration and cause of infertility (female factor includes tubal, endometriosis, hypothalamic, ovarian, uterine, and cervical, male and unexplained factors), type of infertility, type of transfer (fresh or freeze), Hormones level on the day of transfer, thickness of the endometrium on the day of transfer and history of infertility treatment.
Ovarian stimulation protocol for fresh embryo transfer
Yasmin (Bayer) Contraceptive pill started on the third day of menstrual cycle. Flexible antagonist protocol was initiated for the development of multiple follicles using gonadotropin-releasing hormone (GnRh) (MerkSerono frankfurter str. 250, 64293 Darmstadt Germany). Gonadotropin dose was given according to the size of developing follicle and E2 (Estradiol) value. Follicular growth monitoring was done by the gynaecologist using vaginal ultrasound (Wipro GE Healthcare Logiq C5 Premium and Logiq 200). An Ovitrelle 250 micrograms/0.5 ml prefilled syringe (recombinant human chorionic gonadotropin) is administered to trigger final follicular maturation when at least three follicles with a diameter of 18 mm were appeared and luteinisation after stimulation of follicular. Endometrial thickness was measured by transvaginal ultrasound (TVS). Oocyte pickup was performed 34-36 hours after the Ovitrelle injection (Merck Serono Europe Limited) in the operating room under general anaesthesia.
Ovarian stimulation protocol for frozen embryo transfer
In frozen embryo transfer Gonadotropin-releasing hormone (GnRH) agonist, (Lupride Inca Sun Pharmaceutical ltd) (20 U Subcutaneous injection on per day basis) was administered from day 21st of patient’s previous mensuration cycle. Lupride was administered daily to help shut off body’s normal process of hormone and egg development. Following this. Tab estradiolvalerate 2.0 mg (Progynova 2 milligram) was given to patient for uterine lining, embryo implantation and the resulting pregnancy. Low dose progesterone was started when the endometrium thickness reached at least 8mm triple layer CD 3-4 grade then frozen embryo transfer was done under ultrasound guidance.
Process of fertilisation by ICSI
In vitro fertilization (IVF) or Intracytoplasmic sperm injection (ICSI) was performed 4 to 6 hours after OPU. Sperms preparation performed by density gradient method. For some cases we were used the cryopreserved and thaw sperms sample when male partner was not available on same day. We have used ICSI technique for fertilisation. embryo assessment was based on morphology and rate of development. The grade of Day 3 embryos were scored on a scale of 1-4, where 1 and 2 were good embryo, 3-4 were bad embryo. Then we performed Day 3 embryo transfer. We usually transferred 2 or 3 good embryos. All remaining good quality embryos we were cryopreserved through vitrification. For vitrification we were used two solution one was Equilibration solution (SAGE. IVF Inc. a Cooper Surgical company, Trumbull CT 06611 USA) and second was Vitrification Solution (SAGE.IVF Inc. a Cooper Surgical company, Trumbull CT 06611 USA) we were kept the embryo in first solution for 5 minute and 1 minute in second solution. For cryopreservation we were used closed system in that we were kept the embryos on a straw and dip inside the liquid nitrogen straw stored in goblet and goblet were kept in cryocane with appropriate labelling.
When hormones level and patients characteristics like monthly period cycle reach in natural state then we were thaw cryopreserved embryos by using thawing protocol after taking out the straw from goblet and cryocane immediately we were dip this straw in 1.0 M Sucrose warming solution for 1 minute, 0.5 M Sucrose warming solution for 4 minute and Mops solution for 9 minute respectively solution is supplied by (SAGE. IVF Inc. a Cooper surgical company, Trumbull CT 06611 USA). Thaw embryos were transfer to triple layer of uterus when double thickness of endometrium exceeded 8 mm.
Clinical pregnancy was validated by detecting an increased concentration of β-HCG (>25U/ml) 16 days post embryo transfer, and was defined as positive biochemical pregnancy or observed by gestational sac with or without a fetal heartbeat on ultrasound scanning evaluation on 30thday post embryo transfer. The number of sacs was taken as the number of implantations.
Statistical analysis
Statistical comparison was done by using Pie and bar test for representation of categorical value. We were used both the value of fresh embryo transfer and frozen embryo transfer. P<0.05 was considered statistically significant for all measures.
Result
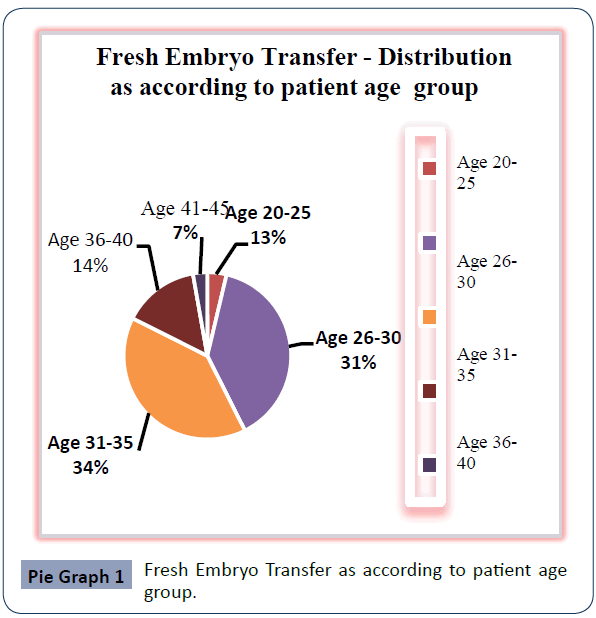
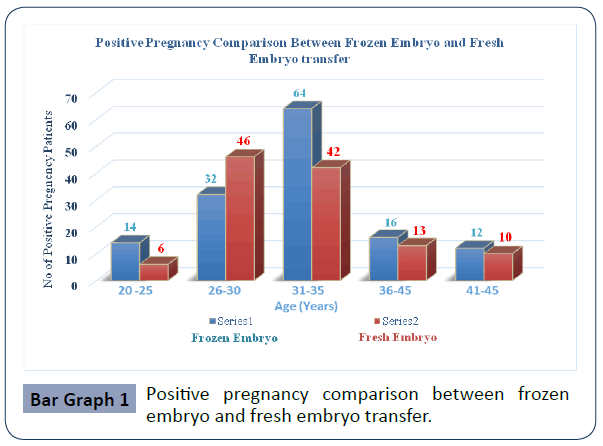
The study concluded that from 210 woman in Fresh embryo transfer group and 222 woman in Frozen- thawed embryo transfer group undergoing ICSI, after analysis of these data frozen – thawed embryo were giving more success in pregnancy out come in the patient age group of 31-45 year. Patients’ distribution and characteristics in these two groups are listed in Pie chart 1, 2 and Bar chart 1. Table I represents the cycle characteristics like fertilised embryo, transferred embryo. The average number of embryos transferred in fresh group was 2.38 ± 1.2 and freezing group was 2.22 ±1.7, Biochemical pregnancy rate was 55.45% in fresh ET group versus 62.16% in FET group. The results between these two groups showed (Bar Graph 1) that frozen – thawed embryo were giving more positive pregnancy rate in patient age group of 31-45 years.
| Fresh Embryo | Frozen Embryo | p -value | |
|---|---|---|---|
| n= 210 | n=222 | ||
| Patient Age | 31.6 ± 9.2 | 32.19 ± 8.9 | 0.757 |
| Expected Oocyte | 12.2 ± 4.1 | 12.36 ± 3.9 | 0.025 |
| Retrieved Oocyte | 13.13 ± 5.4 | 13.09 ± 4.9 | <0.0043 |
| No of Fertilised Embryos | 7.68 ± 6.9 | 8.11 ± 5.4 | <0.0035 |
| No of Embryos Cleaved | 7.01 ± 6.84 | 7.23 ± 6.11 | <0.0038 |
| No of good embryo Transferred | 2.38 ± 1.2 | 2.22 ± 1.7 | <0.0001 |
| Positive Pregnancy | 117/210 | 138/222 | 0.436 |
| Positive Pregnancy % | 55.71% | 62.16% | 0.521 |
Note: Values are presented as number, number (%) or Mean ± SD.
Table I: comparison with fresh embryo transfer and frozen embryo transfer.
Discussion
This systematic study showed a higher clinical pregnancy rate in frozen embryo transfers compare with fresh embryo transfers. This study proved that the cryopreservation of all viable embryos and subsequent FET is associated with improved pregnancy outcomes compared with fresh embryo transfer.
The results favouring FET instead of fresh embryo transfer may be related to the adverse effects of COH on endometrial receptivity, as well as the improved results that can be achieved with current cryopreservation methods [13].
Embryo implantation is one of the important steps for reproductive success, and implantation failure remains an unsolved problem in ART. In two-thirds of the implantation failures, the primary responsible source of failure is the impairment of the ER, whereas the embryo itself is responsible for only one-third of the failures [14]. At the end of the follicular phase in COH, the subtle increases in serum P levels (i.e., premature luteinisation) show a positive correlation with FSH levels, and this increase is associated with an advanced endometrial ultrastructural morphology and echogenicity [15-17].
The cryopreservation of embryos has become a routine procedure in ART when embryo transfer is either impossible or inconvenient. When the FET is performed, the endometrial preparation may be achieved in a natural or an artificial way. It is suggested that during the endometrial priming for FET, the endometrium is more receptive than in fresh embryo cycles [16,17].
Pregnancy rates were significantly higher in the FET group than fresh ET group [18]. Pregnancy rate per ET cycle remained almost fixed over four years: nearly 50 ± 5% for fresh ICSI cycles, and 60 ± 5% for frozen embryo transfer cycles [19]. Pregnancy rate per retrieval diminished each year for fresh cycles [20]. In another study, the implantation, ongoing and clinical pregnancy rates were significantly higher in FET group [21]. Different implantation rates in two groups may reflect distinct endometrial receptivity and better symmetry between embryo and endometrial development in frozen embryo cycles.
To illustrate the similar results in the current study between the fresh and frozen embryo transfers, multiple factors may be considered. The progressive methods of vitrification conclude more survival and better possible development after thawing. There was no relationship between embryo quality and biochemical pregnancy rate before cryopreservation [22,23].
Also, found that according to morphological grading of embryos, biochemical pregnancy was similar in frozen and fresh groups in their study (27%, 22%) [24-27].
Conclusion
Our results of 422 patients showed that frozen embryo transfer can give better pregnancy outcome in 31-45 age group patient. Because by FET we can maintain time gap between the endometrium and embryos transfer. And we can overcome the adverse effects of controlledovarian hyper-stimulation (COH) on ER during ART cycles.
In summary, the results of this analytic study suggest that the implantation, and ongoing pregnancy outcome rates of ART cycles may be improved by performing frozen embryo transfer compared with fresh embryo transfer.
Acknowledgments
We are grateful to Dr SPS Virk Director Virk Fertility Services, Jalandhar, (Punjab) for their scientific advice for completing this study.
References
- Aydiner F, Yetkin CE, Seli E (2010) Perspectives on emerging biomarkers for non-invasive assessment of embryo viability in assisted reproduction. Curr Mol Med 10: 206-215.
- Rashid NA, Lalitkumar S, Lalitkumar PG, Gemzell-Danielsson K (2011) Endometrial receptivity and human embryo implantation. Am J ReprodImmunol 66:23-30.
- Engelmann F (2011) Cryopreservation of embryos: an overview. Methods Mol Biol 710: 155-184.
- Michelmann HW, Nayudu P (2006) Cryopreservation of human embryos. Cell Tissue Bank 7:135-141.
- Levi AJ, Drews MR, Bergh PA, Miller BT, Scott RT (2001) Controlled ovarian hyperstimulation does not adversely affect endometrial receptivity in in vitro fertilization cycles. Fertil Steril 76: 670-674.
- Nardo LG, Bosch E, Lambalk CB, Gelbaya T A (2013) Controlled ovarian hyperstimulation regimens: A review of the available evidence for clinical practice. Produced on behalf of the BFS Policy and Practice Committee. Hum Fertilily 16: 144-150.
- Andersen AN, Witjes H, Gordon K, Mannaerts B (2011) Predictive factors of ovarian response and clinical outcome after IVF/ICSI following a rFSH/GnRH antagonist protocol with or without oral contraceptive pre-treatment. Hum Reprod 26: 3413-3423.
- Roque M, Valle M, Guimarães F, Sampaio M, Geber S (2015) Freeze-all policy: Fresh vs. frozen-thawed embryo transfer. Fertil Steril 103: 1190-1193.
- Shen C, Shu D, Zhao X, Gao Y (2014) Comparison of clinical outcomes between fresh embryo transfers and frozen-thawed embryo transfers. Iran J Reprod Med 12: 409-414.
- Tiitinen A, Halttunen M, Härkki P, Vuoristo P, Hyden-Granskog C (2001) Elective single embryo transfer: the value of cryopreservation. Hum Reprod 16: 1140-1144.
- Evans J, Hannan NJ, Edgell TA, Vollenhoven BJ, Lutjen PJ, et al. (2014) Fresh versus frozen embryo transfer: Backing clinical decisions with scientific and clinical evidence. Hum Reprod Update 20:808-821.
- De Ziegler D, Fanchin R, De Moustier B, Bulletti C (1998) The hormonal control of endometrial receptivity: Estrogen (E2) and progesterone. In: Journal of Reproductive Immunology pp: 149-166.
- Groenewoud ER, Macklon NS, Cohlen BJ (2012) Cryo-thawed embryo transfer: natural versus artificial cycle. A non-inferiority trial. (ANTARCTICA trial). BMC Womens Health 12: 27.
- Cole LA (2012) Hyperglycosylatedh CG and pregnancy failures. J Reprod Immunol 93: 119-122.
- Fanchin R, Righini C, Ayoubi JM, Olivennes F, De Ziegler D, et al. (2011)New look at endometrial echogenicity: Objective computer-assisted measurements predict endometrial receptivity in in vitro fertilization-embryo transfer. FertilSteril74: 274-281.
- Ginther OJ, Bashir ST, Hoffman MM, Beg MA (2013) Endocrinology of number of follicular waves per estrous cycle and contralateral or ipsilateral relationship between corpus luteum and preovulatory follicle in heifers. Domest Anim Endocrinol 45: 64-71.
- De Pergola G, Maldera S, Tartagni M, Pannacciulli N, Loverro G, et al. (2006) Inhibitory effect of obesity on gonadotropin, estradiol, and inhibin B levels in fertile women. Obesity (Silver Spring) 14: 1954-1960.
- Wunsch A, Sonntag B, Simoni M (2007) Polymorphism of the FSH receptor and ovarian response to FSH. Ann Endocrinol (Paris) 68: 160-166.
- Grisendi V, Spada E, Argento C, Plebani M, Milani S, et al. (2014) Age-specific reference values for serum FSH and estradiol levels throughout the reproductive period. GynecolEndocrinol30: 451-455.
- Decleer W, Osmanagaoglu K, Meganck G, Devroey P (2014) Slightly lower incidence of ectopic pregnancies in frozen embryo transfer cycles versus fresh in vitro fertilization-embryo transfer cycles: A retrospective cohort study. Fertil Steril 101: 162-165.
- Gelbaya TA, Nardo LG, Hunter HR, Fitzgerald CT, Horne G, et al. (2006) Cryopreserved-thawed embryo transfer in natural or down-regulated hormonally controlled cycles: A retrospective study. Fertil Steril 85: 603-609.
- HerreroL, Martínez M, Garcia-Velasco JA (2011) Current status of human oocyte and embryo cryopreservation. Curr Opin Obstet Gynecol 23:245-250.
- Balaban B, UrmanB, Ata B, Isiklar A, Larman MG, et al. (2008) A randomized controlled study of human Day 3 embryo cryopreservation by slow freezing or vitrification: Vitrification is associated with higher survival, metabolism and blastocyst formation. In: Human Reproduction pp: 1976-1982.
- Achache H, Revel A (2006) Endometrial receptivity markers, the journey to successful embryo implantation. Hum Reprod Update 12: 731-746.
- Herrero L, Martínez M, Garcia-Velasco JA (2011) Current status of human oocyte and embryo cryopreservation. Curr Opin Obstet Gynecol 23: 245-250.
- Li M, Lin S, Chen Y, Zhu J, Liu P, et al. (2015) Value of transferring embryos that show no evidence of fertilization at the time of fertilization assessment. Fertil Steril 104: 607-611.
- Ubaldi F, Rienzi L, Baroni E, Ferrero S, Iacobelli M, et al. (2004) Cumulative pregnancy rates after transfer of fresh and thawed embryos. In: European Journal of Obstetrics Gynecology and Reproductive Biology.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences