Lemierre Syndrome in Pregnancy Achieved with In Vitro Fertilization
David Prokai, Bennett Gardner, Brian Brost, Louis Weinstein, Erika Johnston-MacAnanny
1Wake Forest Baptist Medical Center, Winston-Salem, North Carolina, USA
2College of Charleston, South Carolina, USA
- *Corresponding Author:
- David Prokai
Wake Forest Baptist Medical Center
Winston-Salem, North Carolina, USA
Tel: +1-336-716-4594
Fax: +1-336-716-6937
E-mail: dprokai@wakehealth.edu
Received date: February 27, 2017; Accepted date: March 27, 2017; Published date: March 29, 2017
Citation: Prokai D, Gardner B, Brost B, Weinstein L, Johnston-MacAnanny E (2017) Lemierre Syndrome in Pregnancy Achieved with in vitro Fertilization. J Reproductive Endocrinol Infert 2017, 2:1. doi: 10.21767/2476-2008.100016
Copyright: © 2017 Prokai D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
This is a case report of a 30-year-old female diagnosed with Lemierre Syndrome in the first trimester of pregnancy that was achieved via in vitro fertilization. Lemierre syndrome is a rare disease characterized by septic thrombophlebitis, usually involving the internal jugular vein (IJV), and typically incited by an oropharyngeal infection. The patient presented at 7 weeks gestation following a three-day history of neck pain, swelling, and restricted movement. Diagnosis was confirmed via MRI by the presence of thrombosis of the IJV and a phlegmon encompassing the retropharyngeal space. Treatment with intravenous antibiotics and anticoagulation resulted in rapid complete recovery. With increasing use of IVF in the United States, provider’s needs to be aware of the possible rare complications associated with hyperestrogenic states that often occur in conjunction with assisted reproductive techniques. A high index of suspicion is needed as complications may initially be asymptomatic and late in onset.
Essentials
• Lemierre Syndrome (LS) is a rare septic thrombophlebitis involving the internal jugular vein
• A pregnant woman was diagnosed with LS after successful in vitro fertilization (IVF)
• Pregnancy, especially following IVF, complicates the diagnosis and management of LS
• Treatment for LS includes antibiotic therapy with consideration of anticoagulation.
Keywords
Lemierre syndrome; Ovarian hyperstimulation syndrome; Pregnancy; Reproductive techniques; Assisted; Thrombophlebitis
Introduction
Lemierre Syndrome (LS), first described in 1936 by Andre Lemierre, is a septic thrombophlebitis affecting the internal jugular vein [1]. It is common for the disease to be preceded by a pharyngeal infection that spreads from the tonsils or peritonsilar space, sinuses, and the middle ear [2]. A retropharyngeal process apparently precipitated this specific case. Anaerobic bacteria, particularly Fusobacteria species, are the most common responsible pathogens. Many cases demonstrate hematologic seeding of bacteria, especially the lungs, brain, pericardium, and solid organs of the abdomen, but septic thrombophlebitis is the classic finding in LS.
The objective of this report is to describe a case of LS in the first trimester of pregnancy that was achieved with assisted reproductive technology. A brief qualitative literature review is presented which illustrates the challenge of diagnosing and treating this disease in pregnancy. The is first case report of LS in a pregnant patient following in vitro fertilization (IVF) We seek to identify a gap in knowledge related to potentially delayed complications related to the hyperestrogenic states that often occur in conjunction with assisted reproductive techniques. With increasing use of IVF in the United States, providers need to maintain a high index of suspicion for thrombotic complications post ovarian stimulation as symptoms may be non-specific and of late in onset.
Background
At the time of Dr. Lemierre’s description of the syndrome that bears his name, the disease was common and devastating. Eighteen of the 20 cases expired in Lemierre’s initial report in 1936 [1]. The current mortality rate ranges from 4% to 18% [3]. Antibiotic treatment of pharyngitis, oral abscesses, sinusitis, and other oropharyngeal infections have made LS a rare occurrence. Contemporary incidence is estimated between 0.6 and 2.3 cases per million, though reports indicate an increase in recent years, possibly due to antibiotic resistance [4].
Anatomic proximity of an infectious source to the parapharynegeal space, rather than a specific microbe or pathophysiologic process, seems to be the key factor in LS. The most common bacteria is Fusobacterium necrophorum [5-8], a gram-negative non-spore forming obligate anaerobe which produces toxins more virulent than most anaerobes [5]. Fusobacterium can aggregate human platelets without causing them to lyse, explaining how these bacteria may incite thrombi formation [9]. Additional causative microbes include Kleibsiella, Bacteroides, Staphylococcus and Streptococcus [4,6]. Exotic etiologies scattered throughout the literature include mononucleosis, intratumoral abscess [10], and forcible oral sex [11]. LS more commonly affects adolescents and young adults compared with older individuals, perhaps because the former demographic group is more frequently subject to pharyngeal infection. In a recent meta-analysis, 71% of cases were aged 10 to 30 years [4].
Case Summary
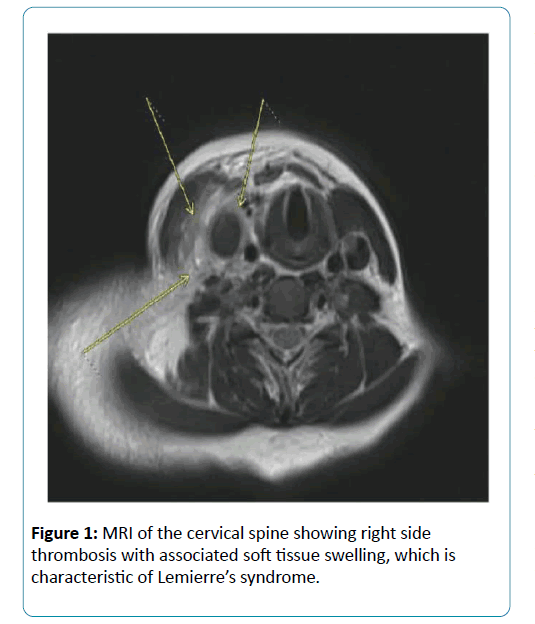
A 30-year-old healthy primigravida presented at seven weeks six days’ gestation with right-sided neck and throat pain, decreased neck mobility and difficulty swallowing. Ultrasound of the right side of the patient’s neck returned positive for a venous thromboembolism (VTE) of the right internal jugular vein (IJV) extending to the right subclavian vein. These findings were corroborated by magnetic resonance imaging (MRI) In addition to VTE, MRI demonstrated a phlegmon encompassing the retropharyngeal and prevertebral spaces, and bilateral pleural effusions (Figure 1). A diagnosis of LS was made based on findings consistent with an infectious process adjacent to the thrombosis of the IJV. The patient was afebrile on presentation and throughout admission. Chest radiograph showed right basilar consolidation and pleural effusion. Laboratory testing returned a WBC of 25,200 and a platelet count of 457,000. Creatinine, electrolytes, and liver function tests returned normal.
Testing for common inherited thrombophilias was positive for a heterozygous Factor V Leiden mutation. Antiphospholipid antibody syndrome assays were negative. Blood cultures returned negative, although they were collected after antibiotic therapy was initiated potentially obscuring culture data.
The patient’s medical and surgical history included tonsiliths, mitral valve regurgitation, appendectomy and a loop electrode excision procedure. Family history was negative for thrombophilia and venous thromboembolism. She underwent assisted reproductive technology for unexplained infertility. Her IVF stimulation was notable for a robust response to gonadotropins with peak estradiol level of 4716 pg/mL. On day of reduced hcg trigger, the patient was started on cabergoline 0.5 mg daily for 8 days. At transvaginal oocyte retrieval, 16 oocytes were retrieved and no ascites was noted. On day of planned embryo transfer, the patient felt well and declined elective single embryo transfer thus two blastocysts were transferred. Three blastocysts were cryopreserved. Single intrauterine pregnancy was noted via ultrasound to have cardiac activity at 7 weeks 5 days gestation, the day prior to the patient’s presentation with LS.
After LS was diagnosed, the patient received intravenous vancomycin and ceftriaxone in the emergency department. Upon admission the infectious disease service discontinued ceftriaxone, adjusted the dosage of vancomycin and began intravenous piperacillin-tazobactam every eight hours. Nasal swab returned negative for MRSA and vancomycin was discontinued. Therapeutic dose enoxaparin at 1 mg/kg twice daily was initiated.
The patient’s symptoms and clinical presentation steadily improved after admission. By discharge on hospital day nine her WBC was 11,300. Repeat MRI prior to discharge demonstrated decreased inflammation of the affected areas and a resolving right-sided pleural effusion. The patient received six weeks of intravenous piperacillin-tazobactam. She continued therapeutic anticoagulation with enoxaparin for the remainder of the pregnancy. The remainder of the pregnancy was without complication and resulted in a term vaginal delivery.
Diagnosis
LS can manifest in a variety of organ systems. Neurologic morbidity is most common (33%), followed by septic arthritis and pulmonary infections 22%) [4]. Other affected sites include the liver, spleen, pericardium, and infections of tissue adjacent to the initial insult. The diversity of the presentations of LS may contribute to the lack of agreed-upon diagnostic criteria [3,12].
A recent case series defined the disease simply as septic thrombophlebitis of the internal jugular vein, eschewing any requirement for specific pathogens, characteristic laboratory findings, or the presence of metastatic thrombi [12]. The patient presented never developed fever or positive blood cultures. However, she exhibited leukocytosis with the MRI findings strongly supporting an infectious etiology in the retropharyngeal space.
The most important prognostic factor in LS is the expediency with which a patient receives a diagnosis and therefore therapy [12,13]. Computed tomography has been the imaging modality of choice due to its sensitivity and ready availability [4,5,12]. Ultrasound may offer a less expensive alternative without the risks associated with exposure to radiation, but this modality lacks the sensitivity of CT [5]. Magnetic resonance imaging (MRI) is relegated to second-line status for most patients [5] while in pregnancy; MRI is an appropriate alternative to CT.
Treatment
The mainstay of treatment for LS is prompt antibiotic therapy with consideration for anticoagulation. Recent sources recommend immediate treatment with intravenous beta-lactam with beta-lactamase and anaerobic coverage [5]. Preferred drugs include ticarcillin-clavulanate, ampicillin-sulbactam, and amoxicillin-clavulanate. Cultures should be used to focus therapy when results become available. Patients should continue intravenous antibiotics at least until resolution of fever and neck tenderness
There is little consensus regarding the role of anticoagulation [3,4,9,12,14]. A recent review conceded the dearth of direct evidence for anticoagulation and advised treatment based on data from “other conditions that involve septic thrombophlebitis”, suggesting that anticoagulation decreases the risk for further thromboembolic events [14]. The authors therefore advocate for anticoagulation in the acute phase of LS with discontinuation once symptoms have resolved.
After careful consideration it was decided to administer longterm anticoagulation therapy for this patient. She had significant risk factors for thrombophilia, including pregnancy and Factor V Leiden heterozygosity. In this context the benefits of anticoagulation throughout the pregnancy and the postpartum period outweighed the risks.
Discussion
Our patient had multiple risk factors for VTE: pregnancy, factor V Leiden heterozygosity (FVL), and history of assisted reproductive technology (ART) Pregnant women heterozygous for FVL comprise about 40% of all VTE in pregnancy [15]. Venous thromboembolism associated with ART demonstrates a predilection for the large vessels of the upper extremities, a phenomenon otherwise rare in pregnancy and for which there is no satisfactory explanation [16]. Women with inherited thrombophilia, such as this patient, may be at elevated risk for VTE of the internal jugular vein when undergoing ART [17]. The case described here is unique in that this patient experienced a rare but well-documented complication of ART-VTE of the internal jugular vein – as a component of an even rarer phenomenon that being LS.
There is one case report of a pregnant woman with LS [6] and one case in a patient during the postpartum period [18]. In the one report of LS in pregnancy, the patient was discharged from the hospital three times before the diagnosis was made [6]. Because of the delay in the diagnosis, she developed septic shock and required mechanical ventilation. In contrast, our patient received a prompt diagnosis and appropriate treatment.
This case illustrates the first known example of LS in a pregnancy achieved using in vitro fertilization. LS is a rare, heterogenous, and serious disease preferentially affecting young adults, including women of childbearing age, requiring all obstetricians to be made aware of this life-threatening disease. Counseling patient who have undergone IVF regarding potential thrombotic complications and their varied symptoms may allow early detection and treatment which avert clinically serious outcomes.
References
- Lemierre A (1936) On certain septicaemias due to anaerobic organisms. The Lancet 227: 701-703.
- Sinave CP, Hardy GJ, Fardy PW (1989) The Lemierre syndrome: suppurative thrombophlebitis of the internal jugular vein secondary to oropharyngeal infection. Medicine 68: 85-94.
- Riordan T (2007) Human infection with Fusobacteriumnecrophorum (Necrobacillosis), with a focus on Lemierre's syndrome. Clinical Microbiology Reviews 20: 622-659.
- Karkos PD, Asrani S, Karkos CD, Leong SC, Theochari EG, et al. (2009) Lemierre's syndrome: A systematic review. The Laryngoscope 119: 1552–1559.
- Golpe R, Marín B, Alonso M (1999) Lemierre's syndrome (necrobacillosis). Postgraduate medical journal 75: 141-144.
- Thompson M, Awonuga AO, Bell J, Ray C, Awonuga MT, et al. (2007) Lemierre's syndrome complicating pregnancy. Infectious diseases in obstetrics and gynecology, 2007.
- Righini CA, Karkas A, Tourniaire R, N'Gouan JM, Schmerber S, et al. (2014) Lemierre syndrome: study of 11 cases and literature review. Head & neck, 36: 1044-1051.
- Agrafiotis M, Moulara E, Chloros D, Tsara V (2015) Lemierre syndrome and the role of modern antibiotics and therapeutic anticoagulation in its treatment. The American journal of emergency medicine, 33: 733-e3.
- Karkos PD, Karkanevatos A, Panagea S, Dingle A, Davies JE (2004) Lemierre's syndrome: how a sore throat can end in disaster. European Journal of Emergency Medicine 11: 228-230.
- Rahhal H, de Campos FPF, Ferreira CR, Felipe-Silva A (2015) Lemierre’s syndrome due to intratumoral abscess of the uvula. Autopsy and Case Reports 5: 11-20.
- Takenouchi S, Kunieda T, Yamada R, Yamakita N (2014) Lemierre syndrome caused by oral sex. Journal of the Formosan Medical Association 113: 762-763.
- Schubert AD, Hotz MA, Caversaccio MD, Arnold A (2015) Septic thrombosis of the internal jugular vein: Lemierre's syndrome revisited. The Laryngoscope 125: 863-868.
- Karkos PD, Karkos CD, Leong SC, Sivaji N, Papadopoulos D, et al. (2010) Lemierre syndrome: no delays in management. The American journal of emergency medicine 28: 844-e1.
- Bondy P, Grant, T (2008) Lemierre's syndrome: what are the roles for anticoagulation and long-term antibiotic therapy? Annals of Otology, Rhinology & Laryngology 117: 679-683.
- American College of Obstetricians and Gynecologists (2013) ACOG Practice Bulletin No. 138. Inherited thrombophilias in pregnancy. ObstetGynecol 122- 706-717.
- van den Broek R, van Balen M, Blaauwgeers J, ten Wolde M (2014) A 28-year-old pregnant woman with a very rare cause of jugular vein thrombosis. Neth J Med 72: 224-226.
- Ergas D, Levin D, Elbirt D, Shelanger H,Sokolovsky N, et al. (2006) Internal jugular vein thrombosis following mild ovarian hyperstimulation syndrome in women with factor V Leiden mutation. American Journal of the Medical Sciences 332: 131.
- McLean AS, Tyler K (1998) Cardiac tamponade in a postpartum woman with Lemierre's syndrome. Anaesthesia and intensive care 26: 582-583.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences