Goserelin vs. Other Treatments in Pain Symptoms Related to Endometriosis after Surgery: An Evidence-Based Case Report
Harzif AK, Handoko Y*, Nanda A, Nilasari D, Nurliana I and Ratna Pratamasari SM
DOI10.36648/2476-2008.2021.6.9
Harzif AK1, Handoko Y2*, Nanda A2, Nilasari D2, Nurliana I2 and Ratna Pratamasari SM2
1Division of Immuno-Endocrinology and Fertility, Department of Obstetrics and Gynecology, Faculty of Medicine Universitas Indonesia, Dr. Cipto Mangunkusumo Hospital Jakarta, Indonesia
2Department of Obstetrics and Gynecology, Faculty of Medicine Universitas Indonesia, Dr. Cipto Mangunkusumo Hospital Jakarta, Indonesia
- *Corresponding Author:
- Yohanes Handoko
Division of Immuno-Endocrinology and Fertility,
Department of Obstetrics and Gynecology,
Faculty of Medicine Universitas Indonesia,
Dr. Cipto Mangunkusumo Hospital,
Diponegoro Street No.71, Jakarta, Indonesia
Tel: +6282210188449
E-mail: yohanes_handoko89@yahoo.co.id
Received Date: September 11, 2018; Accepted Date: January 05, 2019; Published Date: January 12,2019
Citation: Harzif AK, Handoko Y, Nanda A, Nilasari D, Nurliana I, et al. (2019) Goserelin vs. Other Treatments in Pain Symptoms Related to Endometriosis after Surgery: An Evidence-Based Case Report. J Reproductive Endocrinol & Infert. Vol.4 No.1:9
Abstract
Background: The aim of this case study is to know the efficacy of goserelin for pain treatment in endometriosis.
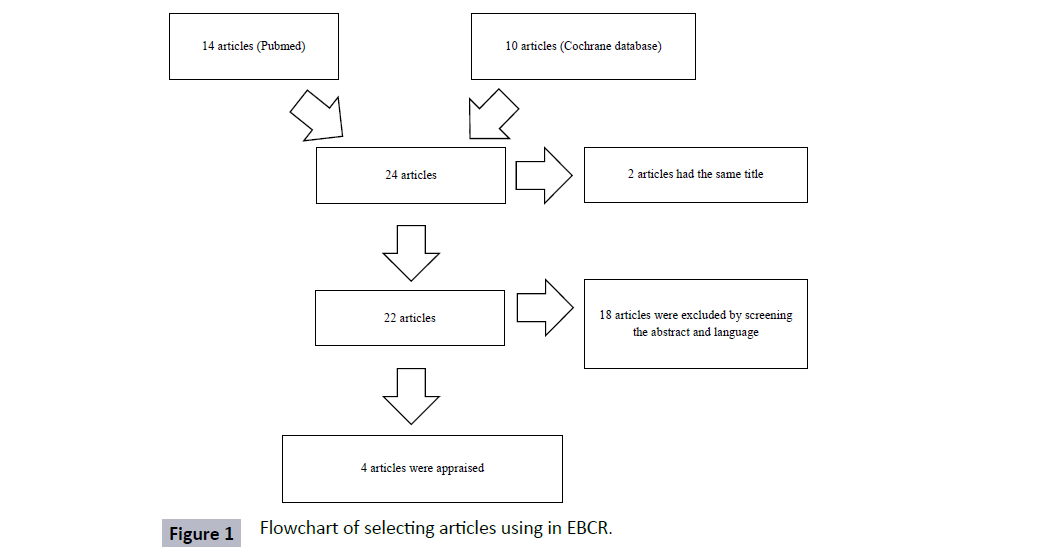
Methods: In this case report, the clinical question is about the treatment of endometriosis, which pain reliever give better outcome to decrease the pain; goserelin or other treatments. To answer this question, we did a searching in PubMed site by using three keywords using MESH, namely ("Goserelin"[Mesh]) and "Pain"[Mesh]) AND "Endometriosis"[Mesh]. Apart from that, we also searched in the Cochrane database by using MeSH descriptor: [Pain] explode all trees AND MeSH descriptor: [Endometriosis] explode all trees AND MeSH descriptor: [Goserelin].
Results: From the searching literature, we found 22 articles which were relevant to the topic. After screening the abstract and language, we got 4 articles to be appraised.
Conclusion: Based on evidences, goserelin was comparable with other treatments. The most common side effect of GnRH was vasomotor symptoms and amenorrhea but that did not reduce patient satisfaction. No serious side effect was observed in goserelin treatment group.
Keywords
Goserelin; Pain; Endometriosis; Adenomyosis; Surgery; GnRH analog; Progestine
Introduction
Endometriosis is characterized by the presence of endometrial tissue in sites other than the uterine cavity and an estrogendependent disorder [1]. Among women in the reproductive age group, estimates of prevalence in the general population are up to 10%. For women with subfertility the prevalence rate ranges from 25% to 40% [1,2]. Pain is universally recognized as the primary complaint of women with endometriosis. This symptom significantly impairs the patient’s quality of life. The management of pain in women with endometriosis has for many years posed a challenge for healthcare professionals [3]. As the pathophysiology of endometriosis is not well understood, its treatment is often unsatisfactory and limited to symptom relief. Treatment options, ranging from / medical therapy (non-surgical intervention) to surgical intervention vary accordingly, as do treatment outcomes. NSAID, GnRH analogues, androgen derivatives, combined oral contraceptives, and progestins are the most commonly used medications in the treatment of endometriosis [4].
There have been 4 studies conducted to know the efficacy of goserelin versus other modalities for treatment of pain associated with endometriosis. However, there is still no formal publication about evidence-based case report (EBCR) discussing about this topic. Furthermore, there is no consensus opinion has been reached in terms of which medication should be used and how long it should be administered. Therefore, we do this analysis to solve the question which often arises during our practice.
The question formulation in this case report study is which one is better to reduce the symptom of pain after surgery in patient with endometriosis. To answer this problem, we do the searching of literature study in this case. Although this report is uncommon on scientific publications in Indonesia, we hope that it can be useful for obstetric and gynecologist specialists to do in their daily practice.
Case History
Mrs. A is 33 years old, working as an employee, with an 8-yearold daughter, and happily married to her husband. Mrs. S has regular menstrual cycle intervals every 28 days, several year history of moderate to severe intensity lower pelvic cramps with heavy flow for about a day (effectively treated with non-steroidal anti-inflammatory agents), recent progressively increasing pelvic and lower back pain that now last for 1-3 days with each cycle (keeping Mrs. S out of work for 2 days a month), and recent diarrhea along with a sharp stabbing pain during urination at the time of her menstrual flow. Seldom, she has post coital pain. Her gynecologist told Mrs. S that she had endometriosis. She underwent laparoscopy procedure 2 weeks ago to treat endometriosis. Her gynecologist planned pain reliever that is suitable for her especially for her menstrual cycle post procedure.
Methods
Formulate the question
For the treatment of endometriosis, which pain reliever give better outcome to decrease the pain; goserelin or other treatments?
Searching the evidences
In order to answer the question above, we did a searching in PubMed site by using three keywords using MESH, namely ("Goserelin"[Mesh]) AND "Pain"[Mesh]) AND "Endometriosis"[Mesh]. Apart from that, we also searched in the Cochrane database by using MeSH descriptor: [Pain] explode all trees AND MeSH descriptor: [Endometriosis] explode all trees AND MeSH descriptor: [Goserelin]. The search strategy identified 22 studies met the inclusion criteria between 1993-2016. From that result, we excluded studies with mandarin language and there were 4 studies could be evaluated (Figure 1).
Results
Appraise the studies
To appraise the scientific evidence of 4 articles, we use the guideline from CONSORT (Consolidated Standard of Reporting Trials) for prospective studies. The tables below describe the appraisal form from the study based on VIA (validity, importance, and applicability) methods (Tables 1 and 2).
Table 1 Validity of the studies included in the analysis.
| Study | Type of study | Focused | Primary outcome | |
|---|---|---|---|---|
| Research question | Selection criteria | |||
| Takaesu et al. [5] | Research article | Yes | Yes | Degrees of menstrual pain and chronic pelvic pain measured by VAS |
| Tekin et al. [6] | Research article | Yes | Yes | Chronic pelvic pain measured by VAS and TESP (total endometriosis severity profile) |
| Vercellini et al. [9] | Research article | Yes | Yes | Pelvic pain measured by verbal rating scale |
| Vercellini et al. [10] | Research article | Yes | Yes | Pelvic pain measured by linear analog and verbal rating scale |
Table 2 Importance of the studies included in the analysis.
| Study | Design of the Studies | Number of subjects | Validity appraisal | Intervention | Duration follow up | Dosage | Outcome |
|---|---|---|---|---|---|---|---|
| Takaesu et al. [5] | Prospective | 111 | Yes | Dienogest vs. goserelin vs. non treatment group | 24 months | Dienogest 2 mg PO for 24 weeks. Goserelin 1.8 mg sub cutaneous once/4 weeks, 6 times. | Improvement in symptom p<0.05 in Dienogest and goserelin group. |
| Tekin et al. [6] | Prospective | 40 | Yes | LNG-IUS vs. GnRH-a | 24 months | GnRH was given every month for 6 months. LNG-IUS: 19-C progestogen (levonorgestrel) 20 µg/day | LNG-IUS: 19-C progestogen (levonorgestrel) 20 µg/day. GnRH: VAS was significantly reduced (p<.001). TESP score showed a significant decrease (P<.001). |
| Vercellini et al. [9] | Prospective | 269 | Yes | Goserelin vs. post-operative expectant management | 6 months | Subcutaneous goserelin depot injections 3.6 mg on six occasions, 28 days apart vs. expectant management | Dysmenorrhoea, alone or associated with other symptoms, was the most frequent moderate or severe event recorded. The cumulative 24-month probabilities of pain recurrence by disease severity in the post-operative medical treatment and surgery only arms were, respectively: 100% and 80% at Stage I; 20% and 48% at Stage II; 13% and 18% at Stage III; and 20% and 23% at Stage IV. |
| Vercellini et al. [10] | Prospective | 57 | Yes | Goserelin vs. EE2 +Desogestrel Pill | 6 months | Goserelin 3.6 mg in a 28 day-subcutaneous depot formulation vs. EE2 0.02 mg+Desogestrel 0.15 mg per pill | Dysmenorrhea (No between group evaluation was performed because of the obvious absence of dysmenorrhea in amenorrhea patients). Dyspareunia (A significant reduction in deep dyspareunia was observed in both groups, with goserelin superior to OC according to linear analog scale (mean difference, 1.8; 95% confidence interval, 0.1 to 3.5). Non Menstrual pain (Non menstrual pain was diminished on both scales without differences between treatments) |
Discussion
Apply the answers
In this EBCR, we appraised 4 studied which fulfilling the inclusion criteria after excluding 22 articles. Critical appraisal was done to randomized control trial study based on VIA (validity, importance, and applicability). A prospective cohort randomized study by Takaesu, administration of dienogest or goserelin was started at the first menstruation after surgery. Dienogest was given 2 mg orally and continued every day for 24 weeks. For goserelin 1.8 mg of subcutaneous injection was given once every 4 weeks a total of six times. Consent for a follow-up study was obtained from patients who desired no postoperative therapy that were assigned into non-treatment group [5].
Menstrual pain was significantly improved during drug administration in both the dienogest and goserelin groups (p<0.05) and also chronic pelvic pain (p<0.05). Menstruation returned at about 3 months after the end of drug administration and then menstrual pain and chronic pelvic pain gradually became worse. In the non-treatment group, menstrual pain and chronic pelvic pain also improved from immediately after the surgery for 6 months, but it was gradually exacerbated after that and showed notable exacerbation as compared with the treatment (p<0.05) [5]. In the non treatment group, menstrual pain and chronic pelvic pain also improved from immediately after the surgery for 6 months, but it was gradually exacerbated after that and showed notable exacerbation as compared with the treatment groups [5]. For coital pain no great improvement was observed in the either of treatment groups or the non-treatment group. The number of subject who had sexual intercourse after surgery was 16 (30%) in dienogest group and 14 (27%) [5].
Other randomized controlled trial compared the effectiveness of levonorgestrel-releasing intrauterine system (LNG-IUS) with GnRH-a treatment on endometriosis related chronic pelvic pain (PCC) [2]. The LNG-IUS delivers levonorgestrel locally, with the result of causing lower systemic progeteron levels, and does not require repeated administration [6,7]. On the other hand the TESP score showed a significant decrease at the first, third, and sixth months of the treatment (P<0.001) in both groups. However, at the final follow-up visit the score was elevated up to the pretreatment levels (P>0.05) in the LNG-IUS group. The lowest levels were detected at the month visit. In the GnRH-a group the TESP score was significantly reduced at the 1-year follow-up (P<0.001) [6].
In the LNG-IUS group, the most common side effects were irregular menstrual bleeding and abdominal pain. Two patients complained of weight gain and in 11 patients simple ovarian cysts were detected, 8 of whom presented with one-sided abdominal pain. None of the patients with ovarian cysts had surgical intervention and the cysts regressed spontaneously. The most common side effects in the GnRH-a group were vasomotor symptoms and amenorrhea, but it did not reduce patient satisfaction [6].
Vercellini et al. [8] compared after surgery the women were assigned to treatment with subcutaneous goserelin depot injections (goserelin) for six months or to expectant management. Post-operative treatment with goserelin significantly prolonged the pain-free interval after conservative surgery for symptomatic endometriosis and did not influence reproductive prognosis. Among the 210 women evaluable for pain recurrence at one-year follow up, 14/107 (1301%) had moderate or severe symptoms in the goserelin group, compared with 22/103 (21.4%) in the expectant management group (P=0.143, Fisher’s exact test), with an observed difference of 8.3% in symptoms recurrence rate (95%CI -2.9% to +19.4%; OR 0-55, 95%CI 0-25 to 1.22) [4].
A open-label randomized trial conducted by Vercellini et al. [9] showed the efficacy of goserelin with a low-dose cyclic oral contraceptive (OC) at the end of treatment and end of follow up with linear analog and verbal rating. For dyspareunia and non-menstrual pain in both goserelin and OC group showed the symptoms improved significantly (p<0.01), with goserelin superior to OC according to the linear analog scale (mean difference, 1.8; 95% confidence interval (CI) 0.1 to 3.5). Women taking OCs experienced a significant reduction in dysmenorrhea on both pain scales (p<0.01) [9].
Assess the outcomes
Our patient with endometriosis experienced with non-steroidal anti-inflammatory agents as pain reliever before surgery. The patient planned to get better drugs to decrease pain caused by endometriosis post-surgery. There are a number of studies about postoperative treatment for endometriosis. However, there is no consensus opinion about which drugs is the best.
Takaesu et al. [5] revealed that significant improvement of symptoms, such as carious pains post-surgery, was observed by drug administration in this report. Recurrence of endometriosis could not be prevented by administration of goserelin as compared with endometriosis without drug administration after the endometriosis was successfully prevented by administration of dienogest. The guideline from the European Society of Human Reproduction and Embryology shows that secondary prevention is defined as interventions to prevent the recurrence of pain symptoms or the recurrence of disease in the long term, which is defined as more than 6 months post-surgery. Hence, dienogest administration could be a first choice to prevent recurrence of endometriosis post-surgery in the future.
Tekin et al. [6] reported that the VAS score had no significant alteration during the follow-up period in the LNG-IUS group, the GnRH-a group showed a significant decrease in the VAS score and endometriosis score at the end of one year. Vercellini et al. [6] revealed that at 6 months of treatment, a significant reduction in deep dyspareunia was observed in both groups, with goserelin superior to the OC at linear analog scale assessment. In 1999, they also reported that post-operative treatment with goserelin significantly prolonged the pain-free interval after conservative surgery for symptomatic endometriosis and did not influence reproductive prognosis [8].
In this evidence-based case report (EBCR), we reported a woman with endometriosis post surgery would like to get pain reliever. She effectively treated with nonsteroidal anti-inflammatory drugs before surgery. From the critical appraisal focused on 4 articles collected from PubMed and Cochrane database with specific criteria, we could summarize that goserelin was comparable with other treatments. The other treatments were dienogest, levonogestrel intra uterine system, oral contraception, and expectant management.
Long-acting GnRH agonists had effect inducing a hypogonadotropic hypogonadal state that had been dubbed pseudomenopause [10]. The most common side effect of GnRH was vasomotor symptoms and amenorrhea but that did not reduce patient satisfaction [6]. No serious side effects were observed in goserelin treatment group in those study [5]. Some concern remains about long term effect of GnRH analogues on bone loss [11]. The decrease in bone mineral associated with standard GnRH agonist treatment regimens (6 months) is significant. Bone loss occurs in both the lumbar spine (trabecular bone) and femoral neck (cortical bone) and can approach or even exceed 1% per month [10].
Conclusion
Based on evidences, goserelin was comparable with other treatments. The most common side effect of GnRH was vasomotor symptoms and amenorrhea but that did not reduce patient satisfaction. No serious side effects were observed in goserelin treatment group.
References
- Brown J, Pan A, Hart RJ (2010) Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. Cochrane Database Syst Rev (12): CD008475.
- Brown J, Farquhar C (2014) Endometriosis: an overview of Cochrane Reviews. Cochrane Database Syst Rev (3): CD009590.
- Cheong YC, Smotra G, Williams AC (2014) Non-surgical interventions for the management of chronic pelvic pain. Cochrane Database Syst Rev (3): CD008797.
- Brown J, Farquhar C (2015) An overview of treatments for endometriosis. JAMA 313: 296-297.
- Takaesu Y, Nishi H, Kojima J Sasaki T, Nagamitsu Y (2016) Dienogest compared with gonadotropin-releasing hormone agonist after conservative surgery for endometriosis. J Obstet Gynaecol Res 42: 1152-1158.
- Tekin YB, Dilbaz B, Altinbas SK (2011) Postoperative medical treatment of chronic pelvic pain related to severe endometriosis: levonorgestrel-releasing intrauterine system versus gonadotropin-releasing hormone analogue. Fertility and Sterility.95: 492-496.
- Kailasam C, Cahill D (2008) Review of the safety, efficacy and patient acceptability of the levonorgestrel-releasing intrauterine system. Patient Preference and Adherence 2: 293-301
- Vercellini P, Crisignani PG, Fadini R (1999) A gonadotrophin-releasinghormone agonist compared with expectant management after conservative surgery for symptomatic endometriosis. J Obstet Gynaecol 106: 672-677
- Vercellini P, Laura Trespidi j, Colombo A, Vendola N, Marchini M, et al. (1993) A gonadotropin-releasing hormone agonist versus a low-dose oral contraceptive for pelvic pain associated with endometriosis. Fertil Steril 60: 75-79.
- Speroff L, Fritz MA (2011) Clinical Gynecologic Endocrinology and Infertility, (8th edn.), Philadelphia, PA USA: Lippincott Williams & Wlikin, Chapter 29: 1221-1249.
- Berek S J, Berek, Novak’s Gynecology (2012) 15th Ed Philadelphia, PA USA: Lippincott Williams & Wilkins Chapter 17.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences